The wide gap between maternal death rates for Black, white mothers persists
By Jimmy Cloutier
Virginia Center for Investigative Journalism at WHRO
As the COVID-19 pandemic has waned with vaccinations and improved treatments, healthcare experts have begun to measure its dramatic effects on expectant and new mothers in Virginia.
Virginia’s maternal mortality rate leaped by 130% during the COVID-19 pandemic, according to an analysis by the Virginia Center for Investigative Journalism at WHRO. In 2021, women in Virginia died of pregnancy-related complications at a rate of 50.1 per 100,000 births, more than double the pre-pandemic rate in 2019, according to data from the National Center for Health Statistics. Virginia mothers died of pregnancy-related complications at a rate of 21.6 per 100,000 births in 2019.
The state also fared poorly compared to the U.S. average of 33 deaths per 100,000 births in 2021. Only Mississippi, Tennessee, Louisiana and Alabama had higher death rates of the 22 states with publicly available data.
Deaths attributed to pregnancy in Virginia are relatively rare, with between 16 and 48 annually between the years 2018 and 2021.
But the alarming spike during the pandemic has experts studying the underlying causes of maternal deaths. Dr. Ryan Diduk-Smith, the Director of the Division of Death Prevention at the Virginia Department of Health, told VCIJ that the state’s maternal mortality review team is just beginning to comb through cases that occurred during the height of the pandemic. Several factors could influence maternal mortality rates, including access to doctors and nurses, delayed appointments and personal decisions about seeking care, she said.
Dr. Donna Hoyert of the National Center for Health Statistics, who authored a recent study on maternal mortality in the U.S., said COVID-19 may have been a contributing factor in maternal deaths. During this time, the rate of maternal deaths in the U.S. increased by roughly 64% — from 20.1 per 100,000 births in 2019 to 32.9 per 100,000 births in 2021.
Maternal mortality rates can vary depending on how they are calculated, with some studies accounting for postpartum deaths occurring within one year of a pregnancy. For this analysis, VCIJ at WHRO duplicated Hoyert’s study, which included only pregnancy-related deaths that occurred during gestation or within 42 days of giving birth.
The results underscore a troubling reality: women face a higher risk of dying from childbirth in Virginia than they do in the U.S. as a whole, and a greater risk than women in developed nations like Canada, Australia and Japan. To be sure, this was true before the pandemic. COVID-19 worsened an already alarming situation.
The data also shows that women of color disproportionately bear the risks associated with childbirth.
Because pregnancy-related deaths are rare relative to deaths from other causes, maternal mortality rates are sensitive to small changes in the total number of deaths and births in a given year, especially when accounting for race. To improve the reliability of Black and white maternal mortality rates, VCIJ at WHRO totaled maternal deaths for multiple years.
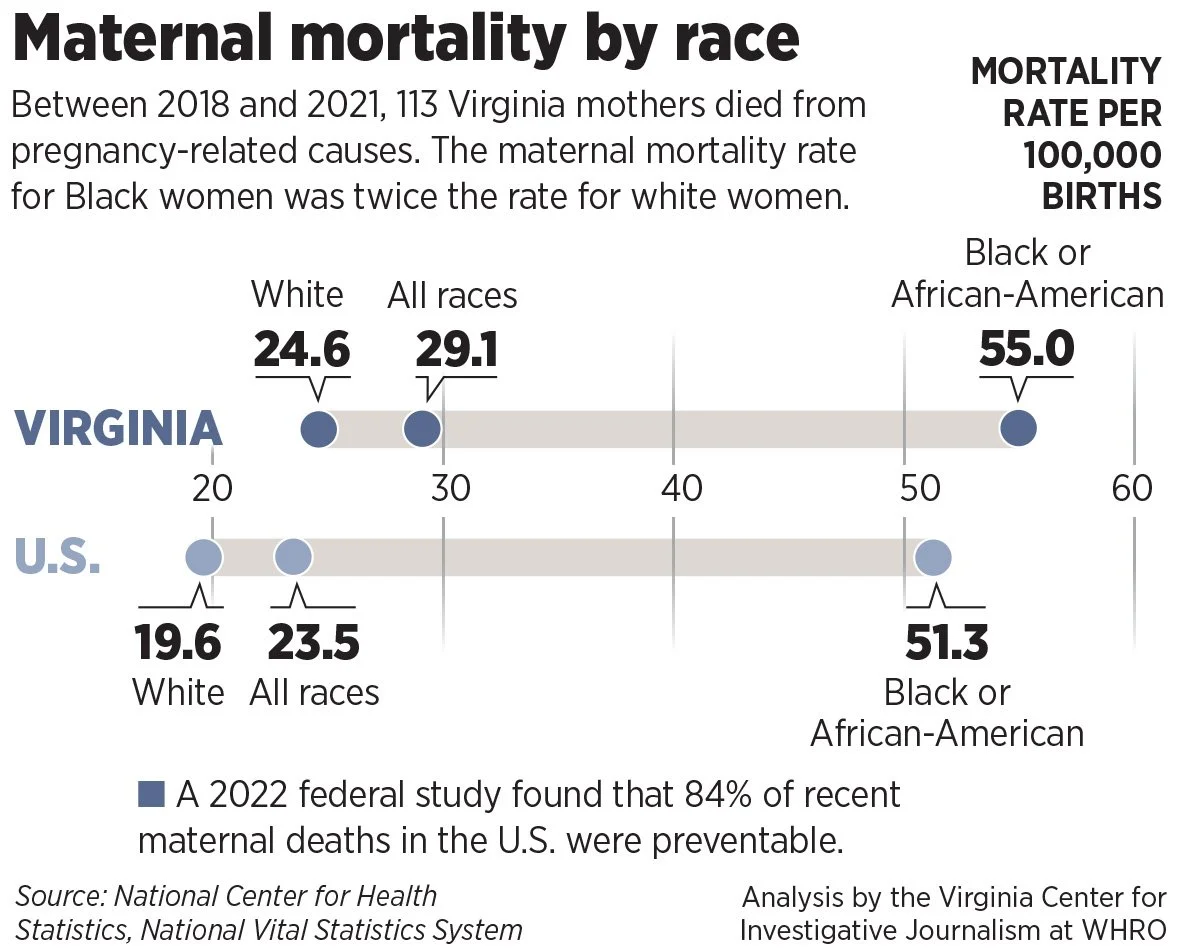
The data shows that between 2018 and 2021, 113 women in Virginia died pregnancy-related causes — a rate of 29.1 per 100,000 births. For Black women, the maternal mortality rate was 55.0 per 100,000 births, more than twice the rate for white women.
These figures are comparable to national maternal mortality rates: Black women in the U.S. died from pregnancy-related complications at a rate of 51.3 per 100,000 births, while white women died from childbirth at a rate of 19.6 per 100,000 births.
Experts are only beginning to understand the circumstances for the racial disparity. A pre-pandemic analysis of 2017-2019 data from maternal mortality review committees in 36 states — including Virginia — found that the leading cause of pregnancy-associated death depended on the race of the mother. The study, which looked at deaths during gestation and within one year of pregnancy, found that the leading cause of death among white women was related to mental health issues. For Black women, the leading cause of death stemmed from cardiac and coronary conditions.
That analysis also found that a staggering 84% of all pregnancy-associated deaths were preventable.
Virginia policymakers have taken steps to improve the quality of maternal data in recent years in an effort to reverse the trend in state maternal mortality. In 2021, the General Assembly established a taskforce to review maternal health data collection. In its first report, released in March, the group proposed that health professionals screen women on mental health, domestic violence, substance abuse and chronic disease during the initial prenatal appointment and postpartum follow up, among other recommendations.
This year’s Virginia Datathon competition, which brings together state agencies, students, nonprofits and the private sector to develop data-driven solutions, is focused on maternal mortality.
Reach Jimmy Cloutier at jrcloutier@proton.me
—
The National Center for Health Statistics notes that states use different criteria for measuring maternal mortality, resulting in underestimates of maternal deaths in some cases and overestimates in others. Experts advise caution when comparing rates between states. VCIJ at WHRO compared Virginia’s maternal mortality rate only to that of the U.S.